Blog
July 2024
Client Testimonial
Are you feeling overwhelmed on your health journey? Same my friend, same! But it doesn’t take tedious tracking or strict [...]
3 Ways To Enhance Health
There is a lot of information these days on how best to fuel your body for different things, including the [...]
June 2024
Cleanse with Kelly this Season
CLEANSE WITH ME THIS SUMMER! As someone with an autoimmune disease, as someone with type 1 diabetes, and as someone with [...]
Type 1 in Midlife Podcast Interview
What an opportunity! I had the best, most welcoming, gentle and inspiring conversation w/ Melissa Stump. Please take the [...]
TrialNet – Type 1 Diabetes Testing
Trialnet offers risk screening and innovative clinical studies to slow or stop T1D, before and soon after diagnosis. ----------- [...]
April 2024
T1D Science Explained: Adjunct Therapies
Below is the content from an email I received from JDRF. I am sharing this information on my blog so [...]
5 Blood Test To Benchmark Every Year
The Importance of Annual Blood Testing for Proactive Health Blood work and advanced medical testing can catch issues before they [...]
January 2024
EMPOWERHER – A New Webinar Series to Empower Women
We have designed this series to empower women to take charge of their health with specific education and recommendations, [...]
November 2023
ENDLESS BLOOD SUGAR TIPS: 2 PASSIONATE DIETITIANS SHARING OUR BEST ADVICE
This week I had the best conversation with a fellow dietitian with a similar mission to help more people flatten [...]
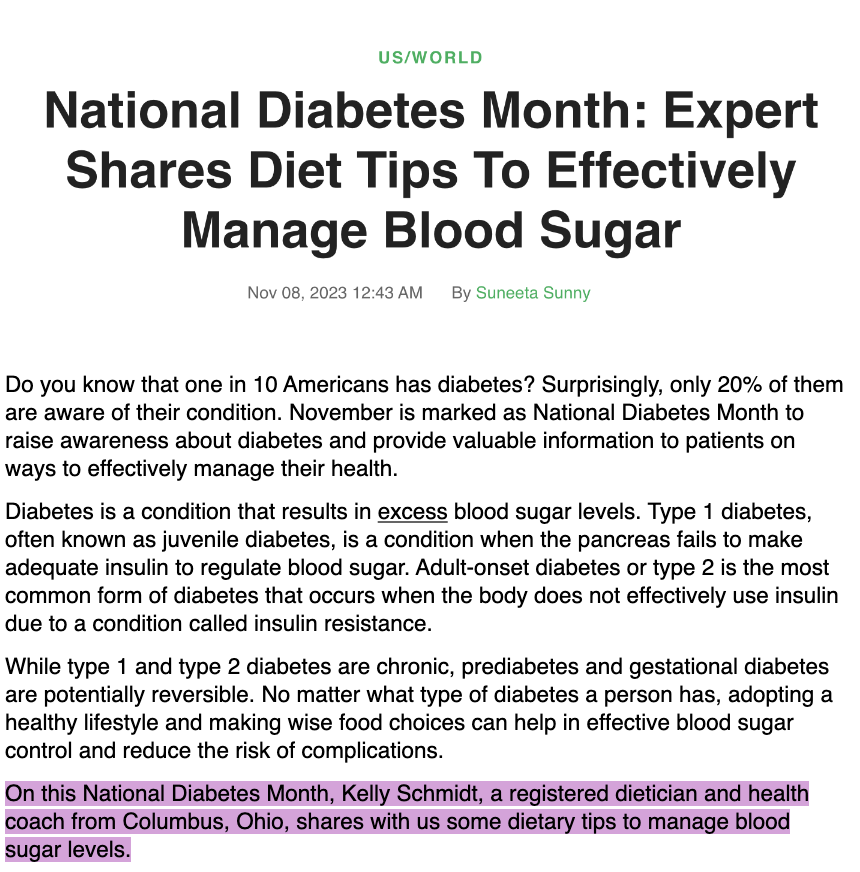
NATIONAL DIABETES MONTH: MY INTERVIEW WITH MEDICAL DAILY
Full read here: https://www.medicaldaily.com/national-diabetes-month-expert-shares-diet-tips-effectively-manage-blood-sugar-471077